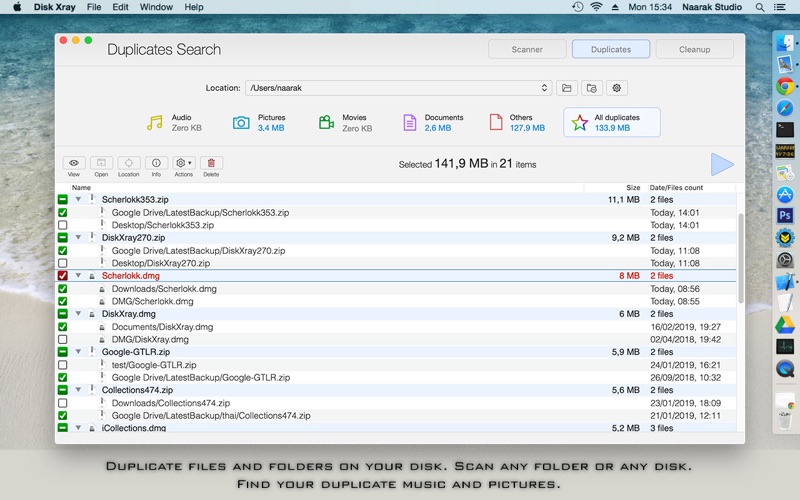
- Disk imaging is the key function of course. Note, that the speed of process and the size of output files are important. For basic understanding, disk imaging is the process of creating an exact copy of a disk for its backup recovery. During it, one large file (usually compressed) is produced, which is later used for recovery process.
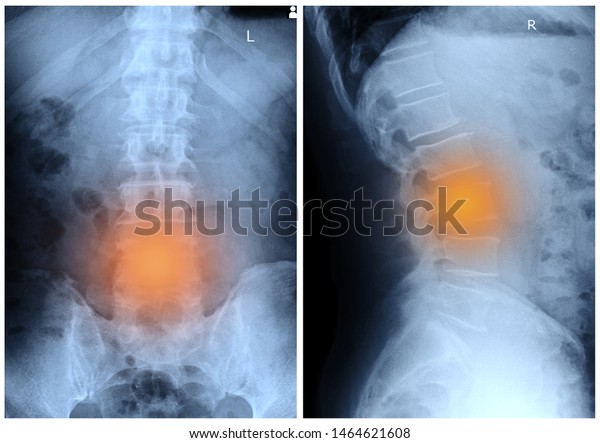
- X-rays of the spine are obtained to search for other potential causes of pain, i.e. Tumors, infections, fractures, etc. Computed tomography scan (CT or CAT scan): A diagnostic image created after a computer reads X-rays; can show the shape and size of the.
- Disc herniation is distinguished from a disc bulge in that it involves less than 25% of the circumference. NB: A number of definitions of what exactly constitutes a disc protrusion have been proposed/used over the years, and it is important to realize that these differ substantially from one another 1-3.
No: a regular X-ray will not show a herniated disc. It may show disc space narrowing which is suggestive of disk disease. A CT may or may not show a her.
Table of Contents
Mnemonic: ABCDEF
How To Open X Rays On Cd
For images of the particular Cervical spine (C-spine) X-ray findings and views mentioned below, please refer to the links at the end of the article or use web-search.
Adequacy
- Skull base, C1-C7 and upper T1 must be visible
- 3 views: True lateral, AP, Odontoid (Open mouth) +/- Swimmer’s view (when a standard lateral view cannot image the cervicothoracic junction)
Alignment
There are lines that must run uninterrupted –
- Lateral view:
- Anterior spinal line
- Posterior spinal line
- Spinolaminar line
- Spinous process tips
- Atlanto-occipital alignment: Anterior margin of foramen magnum should line up with dens (clivus point at dens) and Posterior margin of foramen magnum should line up with C1 spino-laminar line
- A normal dens tilts posteriorly and, if it appears straight or anteriorly tilted, fracture should be considered
- AP view:
- Spinous process line (must be in midline)
- Two lateral lines connecting lateral masses
- Odontoid view:
- Line 1: Make sure lateral masses of C1 doesn’t hang over the lateral masses of C2 (rule of Spence: If combined overhang of lateral masses of C1 over C2 on both sides is >7 mm – transverse ligament injury making Jefferson or C1 ring fracture unstable)
- Line 2: Make sure there is no asymmetry of the articular spaces between the lateral masses of C1 and the body of C2
- Line 3: Make sure there is no asymmetry of the articular spaces between the dens and the lateral masses of C1
Bones
- Trace outline of each vertebral body – below C2 they must be approximately same height and size
- Crushed vertebral body (burst fracture) or flexion deformity with antero-inferior tear drop (tear drop fracture) are unstable
- Trace outline of each pedicle, lateral mass, lamina and spinous process
- Inspect bone density
- Idenitfy “Coffee Bean” shadow – anterior arch of C1 vertebra always visible on lateral view
- Harris ring: Sclerotic ring formed inside body of C2 by it’s lateral masses (break in the ring outline is suggestive of fracture of peg/body of C2)
- Flexion views: >11 degrees angulation using end-plate method and >3.5 mm translation between posterior vertebral lines (anterior translation) is suggestive of mechanical instability
- Forward shift of vertebral body: 25% suggests unilateral facet dislocation and 50% suggests bilateral facet dislocation
- Bow tie sign (Unilateral facet dislocation): bodies appear true lateral below level of injury and oblique above level of injury
- Odontoid view may show odontoid fractures which can be classified by Anderson and D’Alonzo classification:
- Type I – Tip (stable)
- Type II – Odontoid base (unstable)
- Type III – Through body of C2 (stable)
Cartilaginous space
- Pre-dental space or Atlanto-dens interval (ADI): space between odontoid peg and anterior arch of C1 (coffee bean)
- Normal in adults: <3 mm
- Normal in children: <5 mm
Disc and other spaces

- Intervertebral discs: Equal in height at all levels and symmetric and parallel
- Facet joint spaces: Equal distance at all levels
- Spaces between spinous processes:
- C1-C2 space is large
- C3-C7 spaces are similar
- Harris rule of 12: Basion-dental interval (BDI) and Basion-axis interval (BAI) both must be <12 mm (must be </= 8.5 mm on CT)
- Power’s ratio: distance measured from the tip of the basion to the posterior arch of C1 divided by the distance from the opisthion to the anterior arch of C1; >1 is suggestive of occipitocervical dislocation
- Swischuk’s line: A line drawn connecting the anterior cortices of the spinous processes of C1 and C3 should intersect or lie within 1 mm of the anterior cortex of the spinous process of C2. If C2 is >2mm off of this line, it indicates true injury (differentiating from pseudosubluxation)
Degenerative Disk X Ray
Double injuries
Discovery of the most obvious lesion is no reason to drop one’s guard as there may be injury at more than 1 level.
Effusion
- Prevertebral space at C2: <7 mm (< 1/3 vertebral body in children above C4)
- Prevertebral space at C6: <21 mm (<1 vertebral body in children from C4 onwards)
Foreign bodies
Any foreign bodies visible in airway tract
Further reading and pictures:
https://dontforgetthebubbles.com/c-spine-x-ray-interpretation/
https://iem-student.org/how-to-read-c-spine-x-ray/
https://geekymedics.com/cervical-spine-x-ray-interpretation-osce-guide/
He is the section editor of Orthopedics in Epomedicine. He searches for and share simpler ways to make complicated medical topics simple. He also loves writing poetry, listening and playing music.
Herniated disc x-ray films are not an accurate way to diagnose any disc pathology or any soft tissue condition, in general. X-rays are used to image bones and do not detail soft anatomical structures. While x-rays may be useful in determining that some form of disc abnormality exists, it is virtually impossible to determine the exact nature of the disc problem without a more comprehensive visualization test, such as an MRI.
This article will explain why the use of x-rays should not be part of the herniated disc or degenerative disc disease diagnostic processes, despite the fact that narrowed intervertebral spaces can be clearly visualized on x-ray images.
Herniated Disc Diagnosis via X-Ray
Every day, I get letters from patients who say that they were diagnosed with a herniated disc and possibly even a pinched nerve by a doctor or chiropractor who took x-rays. It never ceases to amaze me. X-rays will show a loss of intervertebral disc space, but will usually not be able to determine the cause of the narrowed intervertebral space. After all, there are many reasons for this to occur, ranging from a herniated disc to a ruptured disc to the occurrence of degenerative disc disease.
Normal spinal degeneration or a congenital, genetic or developmental disc abnormality might all look identical on x-ray imaging studies. None of these conditions will be definitively recognizable from an x-ray, nor will their potential effects on the surrounding neurological tissues. The only thing which will be decisively noticed is a lack of typical disc space, with the vertebral bones closer together than would normally occur.
Digital X Ray

X-rays are terrific for imaging osteoarthritic changes, spinal curvatures, spondylolisthesis, fractures and a host of other bone-related concerns. When used for these purposes, x-rays are still a valuable part of the modern diagnostic arsenal. When used to focus on disc abnormalities, x-rays are a complete waste of time, money and offer an unnecessary exposure to dangerous radiation.
Herniated Disc X-Ray Advice
Even though there is a lack of intervertebral disc space noted at a vertebral level, there is no inherent need for concern. Normal spinal degeneration causes this to occur in virtually every human and is especially prevalent in the lower lumbar and cervical spinal regions.
X-rays can not determine which condition is causing this to occur, but will provide the doctor with a reason to order a more detailed test, such as an MRI or CT scan, to better visualize the affected spinal levels. In this regard, x-rays provides a specific purpose. However, x-rays should not be used to make a diagnosis without further and more comprehensive testing via magnetic resonance imaging.
Do not allow any doctor or chiropractor to diagnose a specific disc condition simply based upon x-ray studies. Insist on a better diagnostic tool or find a different doctor who will grant your request for a more comprehensive imaging exam.
Herniated Disc > Herniated Disc Diagnosis > Herniated Disc X-Ray
